Defensible Documentation. Predictable Revenue.
SynchroLink AI resolves the two failures that slow care and revenue: fragmented identity across systems and pre-bill coding that shows insights but doesn’t move dollars.
Patient Identity (EMPI)
One patient, one record—across facilities and EHRs. Beacon identity graph (300M+ profiles), explainable confidence scores, and autonomous merges with human review. Audit trails included.
- 300M+ Beacon identity graph
- Explainable scoring + reason codes
- Autonomous merges + human review
- Audit-ready logs; HIM workload ↓
Pre-Bill RAF & Denial-Prevention
Turn notes, labs, meds, vitals, imaging into audit-ready draft claim lines. MEAT-first, human-in-the-loop, 835 learn-loop to stop repeat denials.
- Accept → Draft with MEAT evidence
- v24 → v28 specificity shown inline
- 835 denial learning to prevent repeats
- Start now—SFTP pilot, CSV/837 out
No MEAT → no draft. Identity and revenue decisions are tied to evidence windows and saved for audit.
Autonomy where it’s safe, review where it matters. Ownership and SLAs keep work calm and accountable.
HIPAA/BAA, encryption in transit & at rest, audit logging, least privilege. Roadmap: SOC 2 → HITRUST.
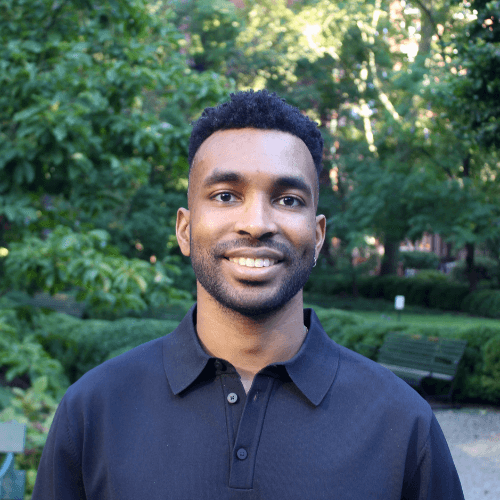
Matthew Harrison
Founder & CEO, SynchroLink AI
 LinkedIn
LinkedInMatthew Harrison grew up in Jamaica, where incomplete medical records often delayed care. That experience shaped his path—from Biomedical Sciences at the University of South Florida into engineering, where he built CTMS, EMRs, LIMS, and patient portals.
Across every system, he saw the same pattern - fragmented patient identity and revenue tools built for dashboards, not action. He founded SynchroLink AI to change that by unifying identity across silos and turning messy clinical evidence into provable, draft claim lines. The goal is simple: trust the record, prove the claim, and get dollars in faster.
Mission - one trusted identity and evidence first revenue so organizations deliver safer care and post real dollars faster.
Fresh insights for risk-bearing teams
Why Risk Adjustment Revenue Is Lost Before Claims Are Ever Submitted
In risk-bearing models, a significant portion of revenue is lost before a claim is ever submitted when documentation exists but doesn’t hold up to encounter-linked, current-year defensibility.
Case Study: Stabilizing RAF With Pre-Bill Documentation Validation
How a value-based care organization reduced late-stage documentation surprises, improved audit readiness, and stabilized RAF by validating defensibility before downstream review cycles locked.
New Insights: The Market Shift Risk-Bearing Orgs Need to React To
ACO REACH turbulence, payer reimbursement drift, and real-time CMS clawbacks are reshaping RAF economics. Here’s how to stay ahead before the dollars disappear.